Overview
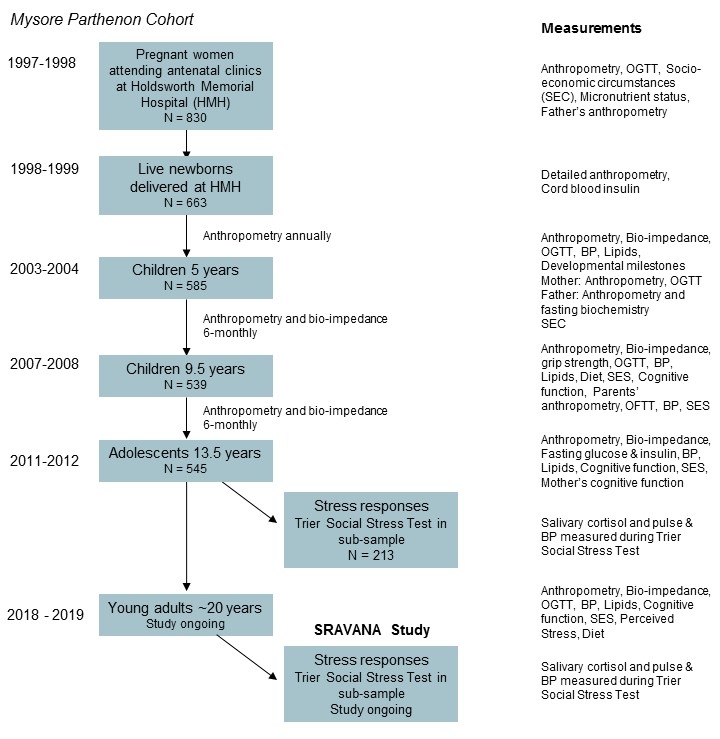
The Mysore Parthenon Cohort Study is led by Dr GV Krishnaveni (Insert image G), Epidemiology Research Unit, CSI Holdsworth Memorial Hospital, Mysore, South India. It was set up prospectively in 1997-8 to assess the prevalence of gestational diabetes (GDM) and its impact on the children. This mainly urban cohort is now aged ~20 years.

Objective
To study associations of GDM, maternal nutrition, newborn size and childhood growth, diet, physical activity and pubertal development with cardiometabolic and cognitive outcomes.
Methods
Women were recruited into the study on booking into the antenatal clinic of the Holdsworth Memorial Hospital. Maternal glucose tolerance and plasma micronutrients (vitamins B12, folate and D) were measured during pregnancy. The children were measured (anthropometry and/or bio-impedance) at birth and every 6-12 months. They and their parents were studied in depth when the children were 5, 9.5 and 13.5 years assessing diet, physical activity, cardiometabolic risk factors and cognitive function. At 13.5 years salivary cortisol and cardiovascular autonomic responses to stress were measured in a sub-sample. The cohort is now aged ~20 years and is currently (2018-2019) taking part in the fourth in-depth round of data collection, including cardiometabolic risk markers and stress responses (SRAVANA study).
Findings from the Mysore Parthenon Cohort study:
- In addition to older age, higher body mass index and a family history of diabetes, lower maternal vitamin B12 status is associated with an increased risk of developing GDM
- Exposure as a fetus to maternal GDM is associated with increased adiposity, hyperglycaemia and hyperinsulinaemia in the children as they grow older
- It is feasible to use the Trier Social Stress Test for Children in a research setting in Indian children and adolescents to measure cortisol and cardiovascular stress responses. Exposure as a fetus to maternal GDM is associated with greater cardiovascular autonomic stress-responsiveness in adolescence compared with children of mothers who did not have GDM
- A conditional analysis, examining the independent associations of the children’s linear growth, adipose tissue gain and lean tissue gain from birth to adolescence with cardiometabolic risk markers in adolescence, shows that it is specifically adipose tissue gain after the age of 2 years that is associated with higher risk (higher insulin resistance and blood pressure)
- A number of early life factors are positively associated with cognitive ability in adolescence, including maternal folate status in pregnancy, newborn size (birth weight and head circumference), childhood height, head circumference and BMI, parents’ educations and the richness of the home environment. Maternal vitamin B12 and D status I pregnancy, and infant feeding method (breastfeeding v formula feeding) were unrelated to the child’s cognitive function
- Dietary assessments have shown that, unlike western populations, data-driven methods such as principal components analysis do not identify clear ‘healthy’ and ‘unhealthy’ children’s diet patterns; their diet patterns were related to socio-cultural factors such as religion and family type (nuclear or joint families) and comprised combinations of both healthy and unhealthy foods, for example high intakes of fried snacks as well as fruit. Children with higher meat and fish intakes, and higher intakes of proprietary malted drinks, which are marketed for children and are high in sugar as well as micronutrient-enriched, had a lower prevalence of vitamin B12 deficiency
Selected recent publications from the Mysore Parthenon Study (with links to Pubmed):
- Kehoe S, Krishnaveni GV, Veena SR, Guntupalli AM, Margetts BM, Fall CHD, Robinson SM. Diet patterns are associated with demographic factors and nutritional status in South Indian children. Maternal and Child Nutrition 2014; 10: 145-58. PMID: 23819872
- Krishnaveni GV, Veena SR, Karat SC, Yajnik CS, Fall CHD. Association between maternal folate concentrations during pregnancy and insulin resistance in Indian children. Diabetologia 2014; 57: 110-121. PMID: 24162586
- Krishnaveni GV, Veena SR, Hill JC, Karat SC Fall CHD. Cohort Profile: Mysore Parthenon Birth Cohort. Int J Epidemiol 2015; 44: 28-36. PMID: 24609067
- Krishnaveni GV, Veena SR, Jones A, Srinivasan K, Osmond C, Karat SC, Kurpad AV, Fall CHD. Exposure to maternal gestational diabetes is associated with higher cardiovascular responses to stress in adolescent Indians. J Clin Endocrinol Metab 2015; 100:986-93. PMID: 25478935
- Christian AM, Krishnaveni GV, Kehoe S, Veena SR, Khanum R, Marley-Zagar E, Edwards P, Margetts BM, Fall CHD. Contribution of Food Sources to the Vitamin B12 Status of South Indian Children from a cohort recruited in the city of Mysore. Public Health Nutrition 2015; 18: 596-609. PMID: 24866058.
- Krishnaveni GV, Veena SR, Srinivasan K, Osmond C, Fall CHD. Linear growth and fat and lean tissue gain during childhood: associations with cardiometabolic and cognitive outcomes in adolescent Indian children. PLoS One 2015; 10: e0143231. PMID: 26575994
- Veena SR, Krishnaveni GV, Srinivasan K, Thajna KP, Hegde BG, Gale CR, Fall CHD. Association between maternal vitamin D status during pregnancy and offspring cognitive function during childhood and adolescence. Asia Pacific J Clin Nutr 2017; 26: 438-449. PMID: 28429909
- Krishnaveni GV, Kumaran K, Krishna M, Sahariah SA, Chandak G, SH Kehoe, Jones A, Bhat D, Danivas V, Srinivasan K, Shanthi JS, Karat SC, Barker M, Osmond C, Yajnik CS, Fall CHD. Life course programming of stress responses in adolescents and young adults in India: Protocol of the Stress Responses in Adolescence and Vulnerability to Adult Non-communicable disease (SRAVANA) Study. Wellcome Open Research 2018 ;3:56. doi: 10.12688/wellcomeopenres. 14583.1. PMID: 30027123
- Di Gravio C, Krishnaveni GV, Somashekara R, Veena SR, Kumaran K, Krishna M, Karat SC, Fall CHD. Comparing BMI with skinfolds to estimate age at adiposity rebound and its associations with cardio-metabolic risk markers in adolescence. Int J Obesity 2018 (e-pub) doi: 10.1038/s41366-018-0144-8. PMID: 30006579
